Abstract
Background: Sickle cell disease (SCD) is a chronic condition characterized by painful vaso-occlusive (VOC) episodes which lead to poor health-related quality of life (HRQL) and premature mortality. As curative treatment with hematopoietic stem cell transplant is only an option for a minority of adult patients, current treatments are palliative with focus on pain management. Clinically, pain assessment is commonly performed by the Numeric Rating Scale (NRS), where patients rate the intensity of pain from 0 (no pain)-10 (worst imaginable pain). However, the incorporation of HRQL through the use of newer patient-reported outcome measures (PROs) into the assessment of pain and the care of patients with SCD is evolving. As these newer measures were developed in ambulatory populations, to date, they have not been studied among adults with SCD hospitalized for painful VOC.
Objective: To describe the VOC pain experience and its effect on HRQL in hospitalized adults with SCD, using two PRO measures, the Patient-Reported Outcomes Measurement Information system (PROMIS) Global Health and the Adult Sickle Cell Quality of Life Measurement System (ASCQ-Me).
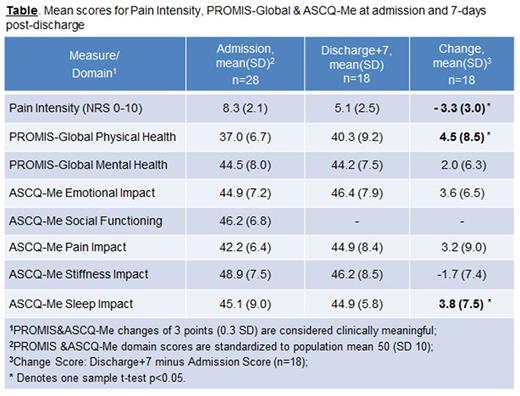
Methods: Adults with SCD hospitalized at a US-based academic medical center with VOC were eligible. Following study enrollment at hospital admission (T1), participants completed the ASCQ-Me Pain Episode assessment, which yields a Frequency score (range 0-11) and Severity score (range 0-22), where higher scores reflect worse disease over the prior year. Participants also complete PROMIS Global and ASCQ-Me at T1. Seven days after hospital discharge (T2), participants again completed PROMIS Global and ASCQ-Me questionnaires. These measures yield scores in domains of global physical and mental health, and SCD-related domains of emotional, social functioning, pain, stiffness, and sleep impact, respectfully. Standardized domain scores have a mean of 50 (SD=10) where higher scores indicate better functioning. Changes of 3 points (0.3 SD) are considered clinically meaningful. We calculated means and standard deviations for the NRS and domain scores at T1 and T2. One sample t-tests were used to compare domain change scores from Admission to Discharge+7, restricted to respondents with complete follow-up.
Results: We report preliminary results from our larger inception cohort. To date, 28 of 29 eligible patients consented and completed T1 assessments (97%). 18 also completed T2 assessments. Of the 10 participants who did not complete T2 assessments, 50% were readmitted within 1 week and 20% within one month; the remainder (n=3) were non-respondents at T2.
The mean age was 30.6 years (SD 9.9) with 57% females and 71% self-identified as black, non-Hispanic. The remainder was Hispanic. The most common genotype was HbSS (57%). T1 mean ASCQ-Me Pain Episode Frequency score was 9 (SD 2.2, range 4-11) and Severity score was 18 (SD 3.1, range 8-22), reflecting recurrent and prolonged painful VOC episodes over the prior year.
At hospital admission, 66% of patients had 4 or more pain crises in the last 12 months. The mean score for the most severe pain during the last pain attack was 8.8 (SD = 1.4) on a scale from 0-10. The most recent pain crisis for 66% of patients lasted at least 1 week; 26% reported crisis lasting longer than 2 weeks.
The table presents mean domain scores at each assessment period and the change scores. All domain scores on ASCQ-Me and PROMIS Global were well below population norms. There was statistically significant and clinically meaningful improvement in pain intensity and the domains of physical health, emotional impact and sleep impact by 7 days after discharge (p<0.05).
Conclusions: Administering both general and disease-specific PROs at the point-of-care is feasible and informative. Among this cohort of hospitalized patients with VOC, baseline ASCQ-Me Pain Episode scores reflect recurrent and prolonged painful VOC episodes over the prior year. All ASCQ-Me domain and PROMIS Global scores were well below population norms, indicating substantial suffering from the multidimensional impact of the VOC pain experience both upon admission and following discharge. Despite the intensity of the patients' condition, we demonstrate successful enrollment (97%) and data collection on admission. 64% data completeness at T2 indicates some degree of non-ignorable missing data, which will be addressed in final data analysis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal